As cases of COVID-19 infection have been confirmed in Namibia some social media users have called for the public naming of infected people.
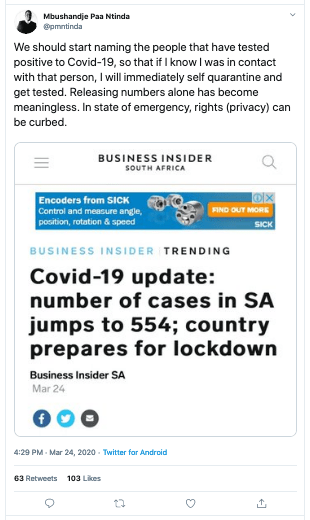
Those in support of the public naming of COVID-19 positive individuals argue that if this information was publicly disclosed, others could put themselves in self-quarantine if they know that they have been in physical contact with infected individuals.
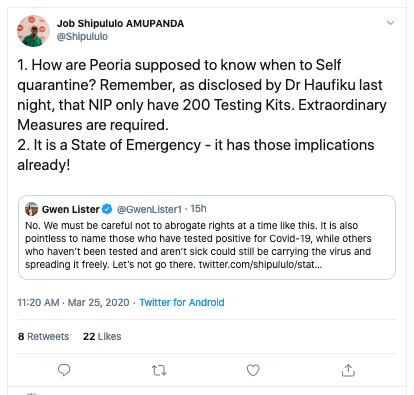
According to those opposing public disclosure of the identities of infected persons, the public naming of individuals who have tested positive for COVID-19 would likely exacerbate public fear, unjustly cast stigma onto individuals and families, and could potentially discourage others from getting tested for the virus, or disclosing a positive test result.
The issue became a hot topic of discussion on Twitter on 24 March 2020, after the following was tweeted:
The topic drew in prominent commentators such as media personality Gwen Lister and Affirmative Repositioning activist Job Amupanda on opposite sides of the debate:
What do the experts say?
Generally, patient-doctor privilege/confidentiality prohibits medical practitioners from sharing information about a patient (such as one’s COVID-19 status) without the explicit consent of the patient, which is similar to attorney-client privilege. It is both a legal and ethical requirement in Namibia and around the world, flowing from the Hippocratic Oath taken by all medical and health practitioners.
According to medicinenet.com, the translated Hippocratic Oath states:
“What I may see or hear in the course of the treatment or even outside of the treatment in regard to the life of men, which on no account one must spread abroad, I will keep to myself, holding such things shameful to be spoken about.”
– Hippocratic Oath
A modern version of the Hippocratic Oath states:
“I will respect the privacy of my patients, for their problems are not disclosed to me that the world may know.”
– Hippocratic Oath
In this regard, the Ethical Guidelines for Health Professionals by the Health Professions Council of Namibia (HPCNA) states:
“Patients have a right to expect that information about them will be held in confidence by the health professional. Confidentiality is central to trust between fellow health professionals and patients. Without assurances about confidentiality, patients may be reluctant to give practitioners the information they need in order to provide good care. If a health professional is asked to provide information about patients, he or she should: (a) Seek patients’ consent to disclosure of information wherever possible, whether or not he or she judges that patients can be identified from the disclosure; (b) Anonymise data where unidentifiable data will serve the purpose; (c) Keep disclosures to the minimum necessary.”
– HPCNA
In a situation where the question becomes whether a public health emergency, such as COVID-19, can allow for a breach of patient confidentiality, the HPCNA states:
“In all such cases the health professional must weigh the possible harm (both to the patient, and the overall trust between practitioners and patients) against the benefits which are likely to arise from the release of information … Ultimately, ‘public interest’ can be determined only by the courts, but the various Health Professions Councils may also require the health professional to justify his or her actions if a complaint is received about the disclosure of personal information without a patient’s consent.”
– HPCNA
In the same vein, Namibia’s Public and Environmental Health Act of 2015 states:
“The chief health officer and a local authority must prevent the spread of a notifiable infectious disease without unnecessarily restricting personal liability or privacy.”
– Public and Environmental Health Act
The law also states a person who suspects or knows that they may have a communicable disease has the right to:
“(i) be protected from unlawful discrimination; and
– Public and Environmental Health Act
(ii) have his or her privacy respected.”
According to a guidance document from the World Health Organisation (WHO) about the rights, roles and responsibilities of health workers during the COVID-19 outbreak, health workers should:
“maintain patient confidentiality;”
– WHO
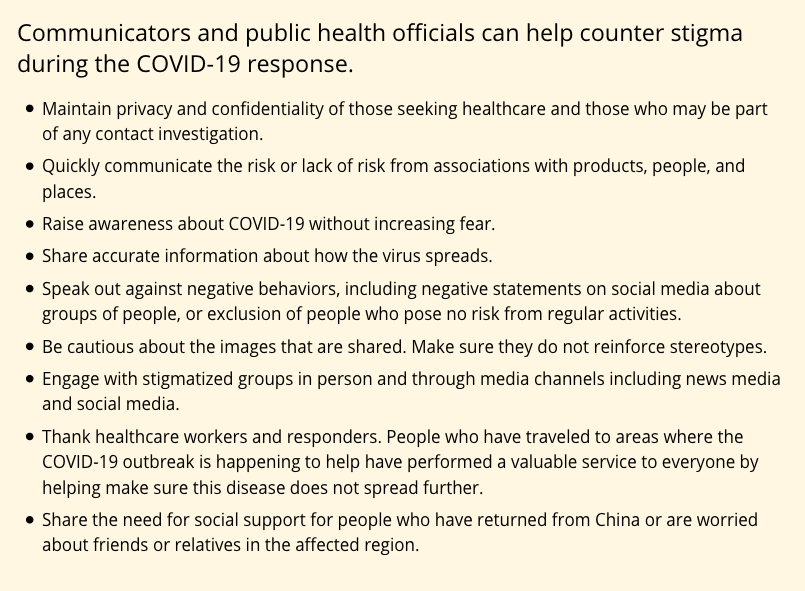
And according to the US’s Centers for Disease Control and Prevention (CDC), maintaining patient confidentiality/privacy is about minimising stigma, and it provides the following guidance: